Cardiac Mapping & Ablation
Cardiac mapping and ablation are advanced medical procedures used to diagnose and treat certain types of heart rhythm disorders (arrhythmias).
What is a Cardiac Mapping & Ablation?
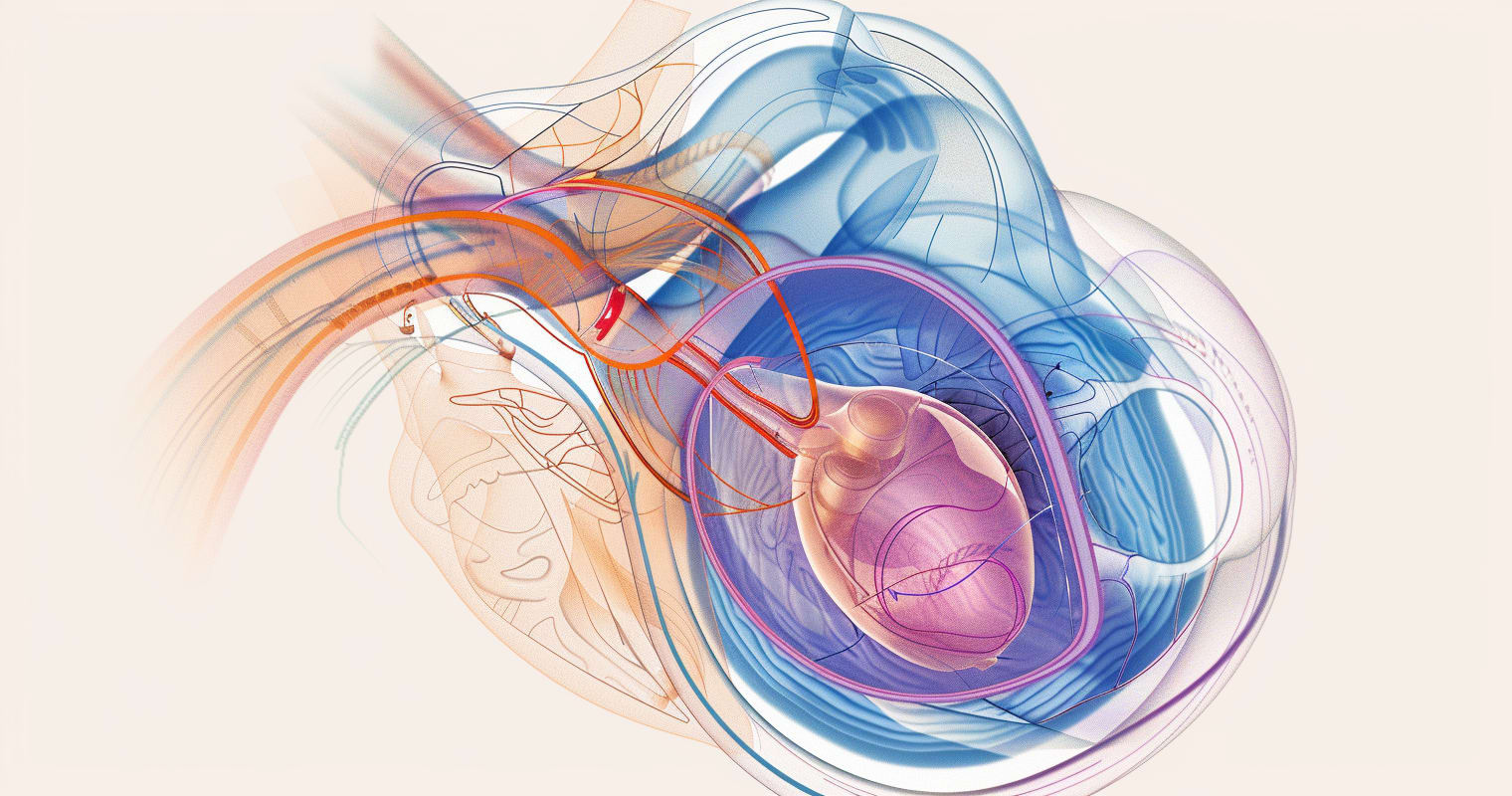
Cardiac Mapping & Ablation is a specialized medical procedure used to diagnose and treat abnormal heart rhythms (arrhythmias). Cardiac mapping is the first phase, where physicians create a detailed map of the heart's electrical activity to identify the abnormal areas causing the arrhythmia. Ablation is the second phase, where these targeted areas are then treated (ablated) to correct the irregular heartbeat. This treatment can be performed using radiofrequency energy (heat) or cryoablation (cold) to create tiny scars in the heart tissue to block the abnormal electrical signals and restore a normal heart rhythm.
Why is the Procedure Performed?
The primary goal of Cardiac Mapping & Ablation is to treat arrhythmias that have not responded to medication or other treatments, or when those treatments are not preferred by the patient. Common types of arrhythmias treated include atrial fibrillation (AFib), atrial flutter, supraventricular tachycardia (SVT), and ventricular tachycardia (VT). This procedure can significantly improve symptoms, such as palpitations, shortness of breath, and fatigue, and enhance the quality of life.
How is the Procedure Performed?
Cardiac Mapping & Ablation is performed in our electrophysiology (EP) lab under sedation determined by your physician. The process involves:
- Catheter Insertion: Thin, flexible tubes (catheters) are inserted through a vein in the groin (or sometimes the neck or arm) and guided to the heart with the help of live X-ray images.
- Mapping: Once the catheters reach the heart, they collect data on the heart's electrical activity to pinpoint the problem areas.
- Ablation: After identifying the problematic tissue, the catheter tips deliver energy (either radiofrequency or cryoenergy) to create small scars that block the abnormal electrical signals.
- Monitoring: The heart's activity is monitored to ensure the arrhythmia is corrected. If the initial ablation does not correct the arrhythmia, the process may be repeated.
What are the Risks and Benefits of the Procedure?
- Benefits:
- Effective treatment for many types of arrhythmias, potentially curing the arrhythmia or significantly reducing its occurrence and severity.
- Improvement in symptoms and quality of life.
- Decreased need for long-term medication use.
- Risks:
- As with any procedure involving the heart, there are risks, though serious complications are rare. These can include bleeding or infection at the catheter insertion site, damage to the heart or blood vessels, blood clots, stroke, and in rare cases, worsening of the arrhythmia or the need for a pacemaker.
- The risk of complications varies based on the individual's health, the type of arrhythmia, and the specific procedure used.
Preparing for Cardiac Mapping & Ablation
What to Expect During the Procedure
- During Cardiac Mapping & Ablation, you will be in a special room called an electrophysiology (EP) lab. You will provided sedation determined by your physician. The procedure can last from 2 to 4 hours, depending on the complexity of your arrhythmia. You will be lying on a table, and monitors will track your heart rate, blood pressure, and oxygen levels.
Pre-op Instructions
- Fasting: You will need to fast (not eat or drink) for 8 hours before the procedure.
- Medication Review: Discuss all medications you are taking with your physician, as some may need to be adjusted or stopped temporarily.
- Pre-Procedure Testing: You may undergo tests, such as blood tests, an EKG, or imaging studies before your procedure.
Medications to Avoid Before the Procedure
- Blood Thinner Medications: You may be asked to stop taking medications, such as blood-thinning medications a few days before the procedure to reduce the risk of bleeding. Do not stop any medications without first consulting your healthcare provider.
- Antiarrhythmic Medications: Depending on the type of arrhythmia, your physician might adjust or temporarily stop your antiarrhythmic medications.
- Other Medications: Inform your physician about all over-the-counter medications, supplements, and herbal treatments you are taking, as some may need to be paused.
- Diabetic Medications: Instructions will be provided on how to adjust or stop insulin or oral hypoglycemics due to fasting.
What to Bring to the Surgery Center
- A List of Medications: Bring a list of your current medications, including doses and how often you take them.
- Personal Items: Wear loose-fitting clothing to the procedure and leave valuables at home.
- Medical Insurance Information: Have your medical insurance card and any necessary medical documents or referrals with you.
What to Expect After the Procedure
- Immediate Post-op: You will be taken to a recovery area to be monitored. You may need to lie flat for several hours to prevent bleeding from the catheter insertion site.
Post-op Instructions
- Activity Restrictions: Avoid strenuous activities and lifting heavy objects for a period of time as advised by your physician.
- Site Care: Keep the catheter insertion site clean and dry. Follow your physician's instructions on how to care for it.
- Medication: You may be prescribed new medications or continue with your previous regimen. It is important to take all medications as directed.
Recovery Tips
- Rest: Ensure you get plenty of rest in the days following the procedure.
- Stay Hydrated: Drink plenty of fluids to help your body recover unless otherwise determined by your physician.
- Healthy Lifestyle: Continue to follow a heart-healthy diet, quit smoking if you smoke, and gradually increase your physical activity as recommended by your healthcare team.
When to Seek Medical Attention
- Emergency Symptoms: If you experience chest pain, difficulty breathing, excessive bleeding or swelling at the catheter insertion site, fever, or signs of infection, seek medical attention immediately.
- Concerns: Contact your physician if you have questions or concerns about your recovery, especially if you notice changes in your heart rhythm or other new symptoms.
Preparing for and understanding what to expect during and after Cardiac Mapping & Ablation can help alleviate any anxiety and ensure a smoother experience and recovery. Always follow your healthcare provider's instructions and do not hesitate to reach out to your medical team with any questions or concerns.
Frequently Asked Questions
Cardiac Catheterization
Cardiac catheterization is a procedure that allows physicians to view your heart by guiding a thin tube through a small incision in the groin or wrist.
Coronary Intervention
Coronary intervention is a type of interventional cardiology procedure to treat blocked blood vessels that supply the heart muscle with oxygen and nutrients.

